Patients who suffer a sudden and unexplained collapsed lung may be better off taking a wait-and-see approach to treatment rather than undergoing surgical intervention, a new study shows.
The research involved 316 people who presented to hospitals in Australia and New Zealand with spontaneous pneumothorax – a collapsed lung that occurs without any obvious cause.
The patients were randomly assigned to either tube insertion in their chests to help their lungs re-expand or simple observation for a minimum of four hours and then sent home provided they did not need oxygen and were walking comfortably.
Both groups were assessed multiple times up to eight weeks following their collapsed lung.
The researchers found 94.6 per cent of the wait-and-see group completely recovered.
For those who had tubes inserted in their chests, the figure was 98.4 per cent. However, these patients were more likely (26 per cent versus 8 per cent) to suffer a serious adverse event, mostly caused by insertion of the chest tube or having the tube in place.
They also were admitted to hospital longer (6.1 days versus 1.6 days) and were more likely to suffer recurrences during the year following their injury.
The researchers admitted the findings were “modest” and “statistically fragile” because of problems in accounting for all patients at their eight-week check-up.
However the New England Journal of Medicine, in which the study was published, said that “with this trial, we can include a conservative approach as a reasonable management option for moderate-to-large pneumothoraxes in otherwise healthy young people.”
Gerben Keijzers, an Adjunct Professor at Bond University and a Senior Emergency Physician at Gold Coast University Hospital (GCUH), is one of the authors of the report.
Professor Keijzers said the study team began to question the traditional treatment of spontaneous pneumothorax because the existing guidelines were based on poor evidence and varied widely between Europe, the US and Australia.
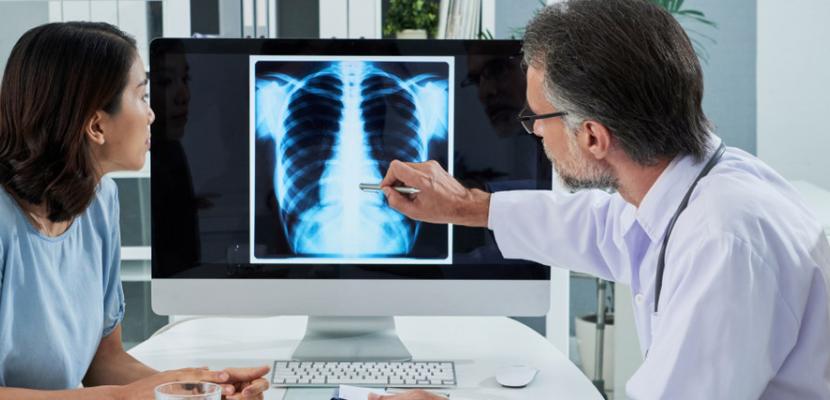
The reason clinicians started inserting drains in the middle of the last century was based on X-rays rather than patients' symptoms.
"The decision for intervention should be based on symptoms rather than the X-ray alone," Professor Keijzers said.
"I think that over the time we conducted this research, both clinicians and patients have become more comfortable with observation, and the study provided further proof to support that doing nothing was safe and reasonable.
"So while there was a group of people already trying to be more conservative, that wasn't widely adopted because the data wasn't quite there."
Professor Keijzers said that as the study unfolded over seven years, doctors and patients at GCUH became more comfortable with the wait-and-see approach.
"When I started with this study probably 80 per cent of our patients (had their collapsed lung) drained," he said.
"We did a recent audit for the last year and 95 percent of our spontaneous pneumothorax patients are now managed conservatively -- so no drain put in.
"We're probably front-runners from that point of view and a lot of hospitals will have still higher levels of intervention.
"When more clinicians realise that it works, that it's safe, and that patients prefer it, practice will change substantially."
GCUH treats about 50 people a year with spontaneous pneumothorax.